Nephrology
PediaWorks and the American Society of Pediatric Nephrology conducted a survey in 2014 to identify and prioritize new devices to treat pediatric kidney disease. The results from 32 respondents follow. All data may be used without permission or restriction. PediaWorks wishes to thank Rainbow Babies and Children’s Hospital, Cincinnati Children’s Hospital and the Sheikh Zayed Institute for Pediatric Surgical Innovation at Children’s National Hospital for providing financial support.
1. Please rank the following in order from most to least needed (lowest score is most desired).
Rank Score Desired Improvements
1 2.9 Access catheters
2 4.6 Non dialyis methods for AKI
3 4.6 PD catheters
4 4.6 CRRT simplification for operators
5 5.1 Automated citrate anticoagulation system for pediatrics
6 5.2 Better filters
7 5.3 CRRT flow rate accuracy
8 6.2 Reduce lab work/blood need/line entries
9 7.0 Technology to allow non-invasive monitoring of hematocrit on CRRT
10 8.5 Better technique to measure intrabdominal pressure
Comments
a. Smaller biocompatible filters for HD and CRRT for smaller children and neonates. Amino acid containing PD dialysate is needed.
b. AKI prevention methods would clearly be most important as it would obviate need to treat AKI. However, this is a long way off. Access issues are most pressing for children, especially smaller children. Without access we can’t even start; with poor access the device stops and the patient doesn’t get the therapy (“what’s your car’s milage at a red light or with a flat tire?”). Current smallest functional catheter is th 7Fr DL acute line – it is not reliable, often kinks, and we can’t place anything smaller than 8Fr for longer term care – further, the 8Fr has too great a distance between the A and V tips; it won’t fit inside of a small baby’s heart. This is the most critical immediate need. The current crop of filters available in the US is an embarrassment. Our Canadian and European colleagues have had more and better options for small children for a decade – meanwhile, we put babies at risk every day and think we are smart for coming up with work-arounds for problems that should be addressed in the factory before they even happen. PD cath options are better than HD cath options but still limited for smallest infants. Conversation with the pediatric surgical specialists will be critical. The rest of it is interesting but really the stuff above is way more important. Children are dying in the US because we haven’t addressed these issues.
c. Whereas we need improvements in catheters, filters, and CRRT machines, it would be ideal to have non-dialytic therapies for AKI, especially in the very small (<3kg) and hemodynamically unstable patients.
d. Preventing the need for dialysis with meds such as rasburicase is needed.
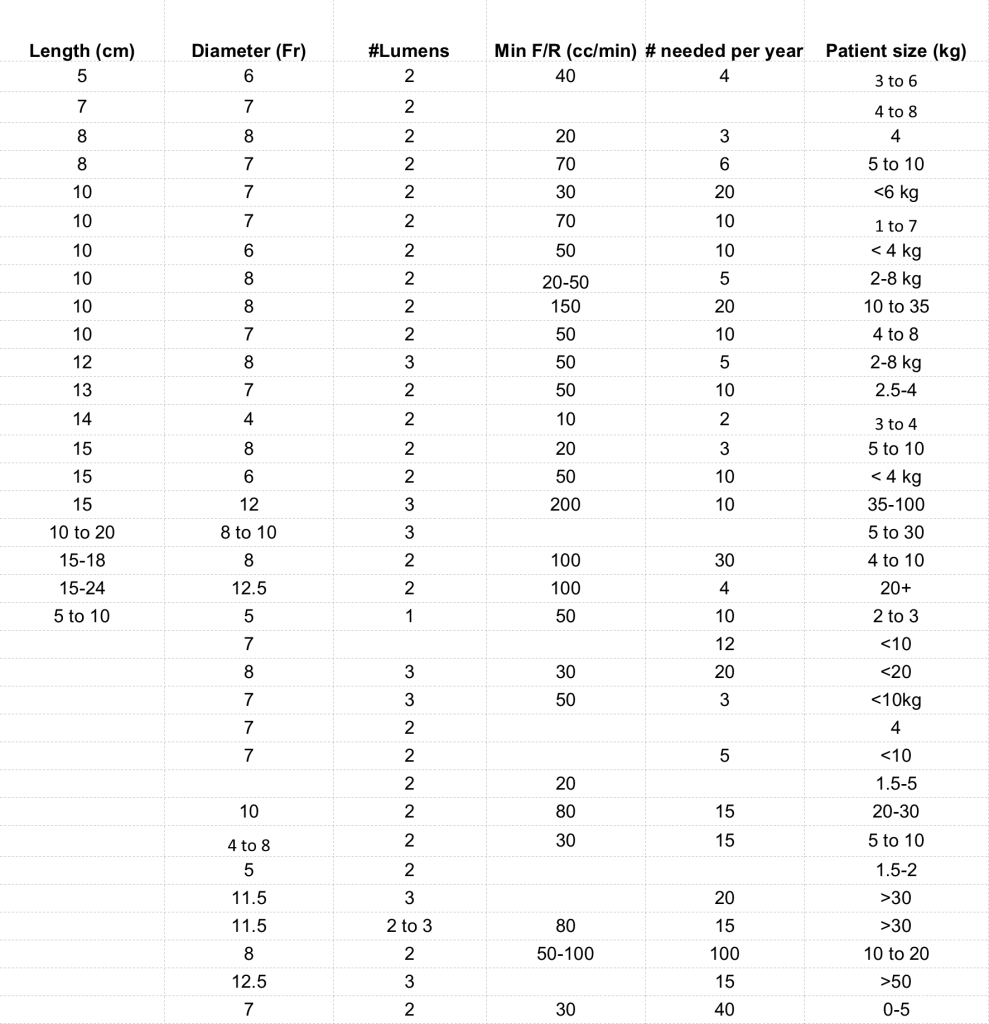
2. Please define the attributes of needed access catheters. Each row is a single catheter.
Comments
a. Access catheters for HD/CRRT are too long for neonates and often problematic to place/use. Need different length catheters. Having a separate lumen for central infusions may be helpful, esp when access is difficult. The distance between the arterial and venous end of the catheter needs to be closer together as the right atrium is smaller in a child.
b. The trouble is often with lack of various catheter lengths for a given diameter as our patients come in many sizes and shapes leading to incorrect position or extruded cuffs.
c. The two catheters first noted above need to be “permanent” catheters with the capability of IJ placement and tunneling for longer-term use. Internal tip displacement between A and V needs to be small enough so that it will work inside a baby’s heart. Cath 3 is the single-lumen acute cath for tinier babies in whom it is too challenging to get the double due to small vessel size.
d. We are at a loss for dual-lumen catheters for the smallest infants, requiring use of multiple single-lumen catheters, especially if we want to use CRRT with calcium/citrate. We also need smaller triple-lumen catheters for CRRT with calcium/citrate, as the only one currently available is 12 Fr. Patients who need CRRT are often extremely ill, and already using every available CVL, so using a separate central line lumen for calcium alone is problematic.
e. No 6 fr available now. the 7 fr medcomp kinks and has memory of kink – does not work more than 1-2 runs usually.
f. Need a triple lumen 8 fr
g. A general comment for all paediatric HD catheters is that we need more flexibility on length – the body growth/dysmorphic issues in many of our kids makes the choice of lumen size to length one where we end up with super long catheters that exit at poor positions – or we end up with a short catheter that has the appropriate lumen. Also much of the hardware is very HEAVY in younger kids, and finally the cuffs being used often do NOT knit properly in an active child. My proposal would be to use Tesio type tech – so each line could be shortened on the table, and the cuffs would be Tesio type as well use lighter hardware pieces – e.g. the blood line connector/ hubs.
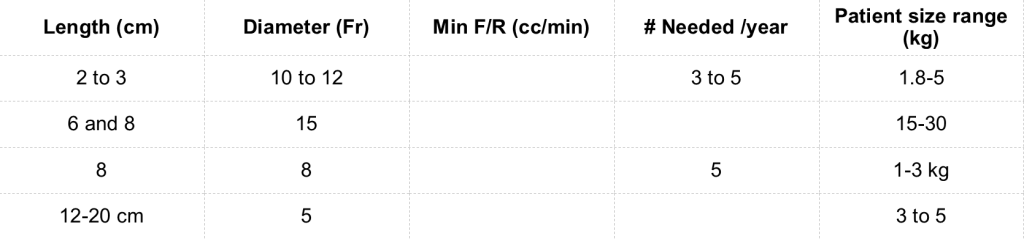
3. Please define the attributes of needed acute PD catheters. Each row is a single catheter.
Comments
a. We hardly ever do acute PD which is a shame
b. More options for neonates
c. More neonatal and infant sizes.
e. We only use permanent PD catheters.
f. The issue with PD catheters is a greater variety of straight vs. curl, # of cuffs, etc. We already have some good options but the surgeons need to weigh in regarding the current complications and how to mitigate.
h. We currently use an 8.5-Fr uncuffed pleural-pericardial pigtail catheter for acute PD in infants with anasarca, replacing the catheter with a Tenckhoff when the abdominal wall edema subsides and the catheter starts to leak. We previously used 5 or 8-Fr pericardiocentesis catheters for this, but they apparently were redesigned and have not functioned successfully in the past 1-2 years. Smaller uncuffed, pigtail PD catheters for short-term acute PD in small infants would avoid the need to surgically place a cuffed catheter, and would allow us to use catheters designed for their intended use.
i. Crucial piece is the distance from the peritoneal cuff to the lowest point. Really need only a premie straight catheter – existing stuff ok otherwise
j. Curled PD catheter for infant (not sure about exact size specifications)
k. Need the shorter length catheters – e.g. cuff to the bottom of the curl as it sits in the pelvis. For the small babies – i.e.
4. Please describe needed access and equipment protocols in order of importance for children on PD, HD or CRRT between 5 and 10 kg.
a. PD and HD access catheters – smaller sizes, appropriate lengths
b. PD cylclers that can deliver a smaller volume
c. PD or CRRT rarely iHD
d. Low flow CRRT with minimal effort to set up- no blood priming
e. Appropriate 8Fr acute and cuffed HD catheters for immediate and longer-term vascular access, designed for kids (not small adults)
f. Combined use of CRRT and ECMO
g. Standards for PD cath placement
h. Shorter HD/CRRT catheters
i. CRRT filter that wont cause bradykinin release syndrome
j. PD – we need the smaller catheter lengths – and preferably curl and straight catheter options with the choice to place a second cuff.
smaller circuits, smaller access.
k. Smaller filter sets for CRRT (biocompatible, polysulphone)
l. Smallest possible blood volume
m. Consistent PD kits for smaler children (better than GESCO sets)
n. Lowest volume tubing sets and hemofilters/dialyzers to limit extracorporeal volume and need for blood priming
o. Alternative anticoagulation protocols in the face of nationwide shortages of calcium
p. Smaller filter/tubing for CRRT (using non AN69 membranes) tubing/filter that allow minimization of extracorporeal blood volume for CRRT/HD in infants
q. PD – we absolutely need better cyclers that have smaller dead space loss and can more accurately handle dwell volumes of 50-100 cc; below 100-120 cc these machines simply don’t work consistently enough and so these kids are often forced to live in hospital till the volumes reach 100++
r. CRRT machines with ability to adjust flow rates in smaller increment
s. Blood warming
t. Hemofilter membrane materials that do not put the patient at risk (e.g. for bradykinin release)
u. Strategies to address hypophosphatemia in patients on CRRT in the face of nationwide shortages of phosphate
v. CRRT machine software that can expect lower blood flow rates
w. HD – WE MUST PRESERVE NEONATAL AND PEDIATRIC LINE SETS AND LIMIT THE EXTRACORPOREAL LINE VOLUMES! Despite smaller high flux dialyzers it is soon going to be true that most HD machines will have as the smallest line set option something that is OVER 100 cc of blood – severely restricting our option to chronically dialyze without blood primes in babies less than 8 or even potentially 10 kg. There is no more pressing issue in paediatric dialysis in my opinion than preservation of equipment that is set up to dialyze babies and children less than 10-15 kg.
x. HD lines (tubing) that are larger than the 2.6 mm neonatal lines, but smaller than the adult 6.35 mm lines
y. Reduce blood flow to 20 ml/min
z. Highly accurate UF control
5. Please describe needed access and equipment protocols in order of importance for children on PD, HD or CRRT between 11 and 20 kg.
a. PD and HD access catheters – smaller sizes, appropriate lengths
b. Not as pressing- can adapt machinery to this relatively easily
c. 8-10Fr lines
d. Smaller filter/tubing for CRRT (using non AN69 membranes)
f. 9 French chronic HD catheter (I think the 9 FR is currently only available as an acute catheter?)
g. Triple lumen 10 f catheter would be nice.
6. Please describe needed access and equipment protocols in order of importance for children on PD, HD or CRRT between 11 and 20 kg.
a. 8-10Fr lines
b. 9French chronic HD catheter (I think the 9 FR is currently only available as an acute catheter?)
c. PD and HD access catheters – smaller sizes, appropriate lengths
d. Same as above
e. Smaller filter/tubing for CRRT (using non AN69 membranes)
f. Not as pressing- can adapt machinery to this relatively easily
g. Triple lumen 10 f catheter would be nice…
h. Acute PD catheters of appropriate size
i. Blood flow can be 30-40 ml/min
j. Smaller filter sets for CRRT (biocompatible, polysulphone)
k. otherwise as above for smaller kids
l. CRRT machine software that can expect lower blood flow rates
m. CRRT machines with ability to adjust flow rates in smaller increaments
n. HD lines (tubing) that are larger than the 2.6 mm neonatal lines, but smaller than the adult 6.35 mm lines
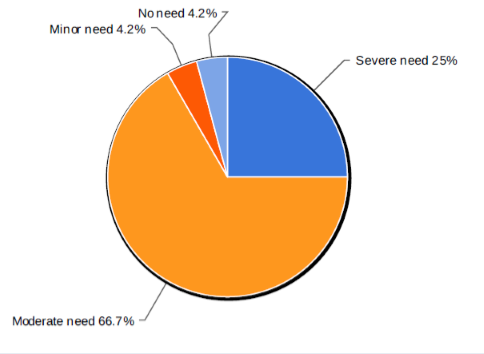
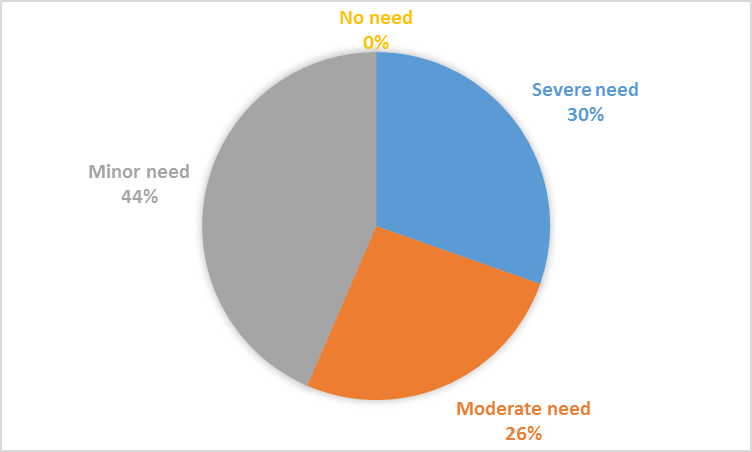
7. Please rate the need for non dialytic therapies of AKI in children less than 5 kg. List the limiting factors in the comments box.
Comments
a. Lots of sick kids, lots of cardiac babies! This population continues to grow
b. No current treatments- need to prevent AKI
c. Perception likely depends on practice location
d. Inherent challenge of vascular access that would allow flows compatible with current machines. PD can be unfeasible in infants with NEC or other abdominal anomalies more so in the post open heart surgery the vascular surgery inserted PD catherters are not leak proof and often used as a “drain”
e. Dialysis access, equipment, and staff may not be readily available for these infants, and avoiding the not insignificant risks of RRT warrant development of non-dialytic therapies especially for this extremely vulnerable population
f. We sometimes have kids this size or smaller for whom we can’t provide successful RRT due to the technical challenges. While I really do need the equipment to save these kids, it would be better not to have to use RRT at all. Prevention and/or non-invasive therapy is always preferred.
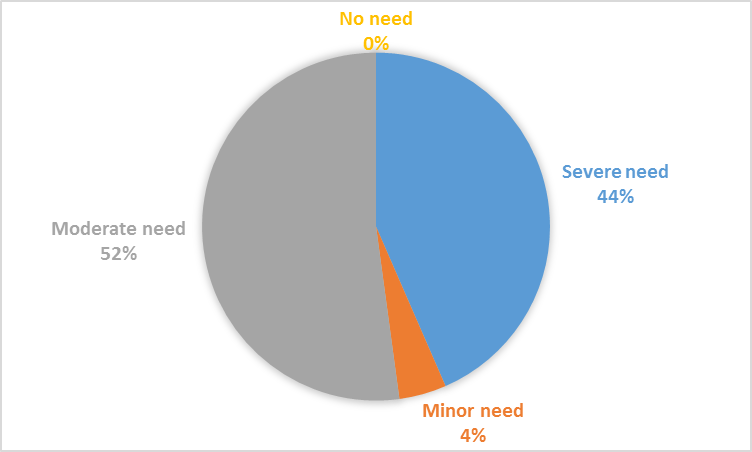
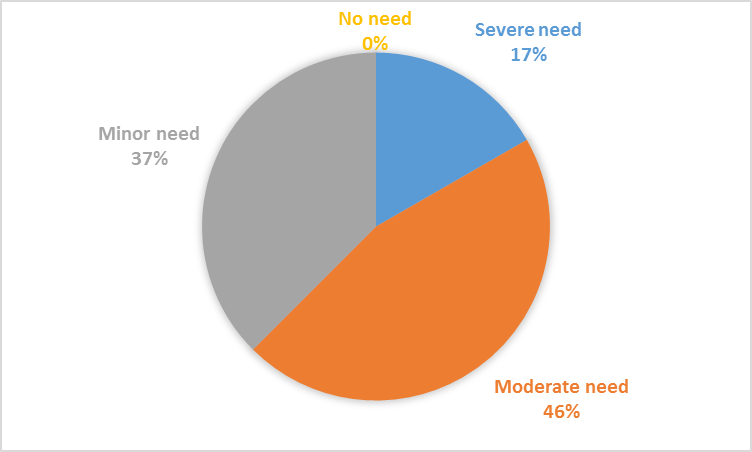
8. Please rate the need for CRRT in children less than 5 kg. List the limiting factors in the comments box.
Comments
a. Again, depends on practice location
b. Extracorporeal volume and bradykinin release with AN69 dialyzer
c. Must reduce minimum blood flow down to 20 ml/min
d. Size of infant, size of catheter, need for blood prime
e. Blood flow rate. vascular access. high pressures encountered.
f. Blood priming access machinery
g. The equipment is all designed to work on a person who weights 60-80kg. Babies die every day because we can’t provide the therapy safely or well – sometimes, we don’t even try because it’s “beyond our capabilities”. Unacceptable.
h. Current Prismaflex polysufone filter sets are too large and unsafe for children under 5 kg. Flow rates on the Primaflex cannot be adjusted in small increments needed for smaller children.
i. Coagulation, accurate blood flow and overall monitoring of parameters, non-invasive monitoring of dia-filtration efficacy
j. Whereas CRRT may be the ideal modality, especially for hemodynamically unstable infants, they may be candidates for acute PD or HD.
9. Please rate the need for CRRT in children less than 3 kg. List the limiting factors in the comments box.
Comments
a. ACCESS MACHINERY Complexity of set up
b. Issues as in #8, but even more critical.
c. Not an area of my practice
d. Size of infant, size of catheter, need for blood prime
e. Blood flow rate. vascular access. high pressures encountered.
f. This is smaller subcategory of ? 8.
g. Same answer as above, but also major difficulty with blood access catheters.
i. Uncommon to need this (typically only need CRRT on neonates on ECMO although that is somewhat institutional dependent.
j. Probably the best modality for hemodynamically unstable infants for whom PD is not an option, but the limitations include access, appropriate filters, need for more precise devices to deliver accurate flow rates, and need for highly skilled staff
k. See comments above box 8 – except for this group, even more likely that folks won’t even try. We know what to do – we just need the tools.
l. Limiting factors that won’t be overcome is usual other system illness severity that complicates treating these kids, other include access and equipment
10. Please rate the need for PD in children less than 2 kg. List the limiting factors in the comments box.
Comments
a. Catheters adequate consistently functional molded sets
b. Size of infant, size of catheter, can only perform manual dialysis only
c. Smaller catheters to prevent skin breakdown
d. Uncommon need. Not really any PD catheters commercially available for these patients.
catheter size/length.
e. Uncommon but difficult technically to do when needed.
f. Need smaller catheters. Better closed, sterile system for doing manual PD. Smaller sets that allow for smaller fill volumes on the cycler
g. Technical – catheter size Personal – poor healing, lack of SQ tissue, leaks, hernias, ect and poor outcomes.
h. I would say anything
i. Need smaller diameter cuffed catheters with a wider range of lengths. Uncuffed catheters addressed above
j. If we can’t do HD or CRRT, we need something else – PD is it. Some babies slowly die because we don’t have the tools – it is so frustrating and it doesn’t have to be this way.
11. Please describe required filter improvements in order of importance.
a. Avoidance of kinin-release syndrome
b. Lowest possible blood volume.
c. Pediatric non-AN69 CRRT membranes
d. Polysulfone is better than AN69
e. Biocompatible smaller filters for smaller children
f. Less bradykinin reaction
g. Low volume effective clearance and no hypotensive reactions
h. See above. CRRT filter that doesn’t cause bradykinin release syndrome
i. Smaller filters and tubing
j. Smaller volume
k. Need better larger molecular molecule clearances – protein/B2 micro globulin in even the smaller surface areas
l. Smallest possible extracorporeal volume to eliminate blood priming (this includes the tubing set!!)
m. Minimizing priming volumes to limit exposure to blood products
n. No bradykinin release syndrome
o. Safer membrane materials that do not cause reactions
p. Wider range of sizes
q. Less prone to clotting, especially in patients with high levels of cytokines
r. Reduced thrombogenicity to simplify (eliminate?) anticoagulation needs
s. Steam sterilization as a standard
t. We no have great baby sized high flux and high efficiency dialyzers in very small surface areas, but would be nice to see more work on clearance of the heavier molecules even in the smaller surface area dialzyers – e.g. PO4 and B2 Microglobulin etc
12. Please describe required CRRT improvements in order of importance.
a. Decreased extracorporeal blood volume requirement
b. Lower blood flow rate
c. More precise flow rates (blood, PBP solution, dialysate)
e. Pediatric non-AN69 CRRT membranes (smaller extracorporeal volume)
f. Peds tubing set
g. Access improvement
h. Simpler equipment to operate
i. Smaller biocompatible (polysulfone or similar) filter sets (a range) for smaller children
j. Smaller filter sizes
k. Smaller filters and tubing
l. Software and UF control systems that operate accurately and reliably at the low volumes needed for children
m. Ability to operate/adjust CRRT with slower blood flow rates and more precision
n. CRRT machine software updates that allows expectation of lower flow rates
o. Lower blood volume
p. More precise UF volume
q. Easier to do an intermittent therapy
r. Flow requirements
s. Machine that has volumetric system rather than scales for measuring fluid flow rates
t. Smaller priming volumes
u. Automated data recording (i.e., the device talks to the electronic medical record – let the nurse take care of the patient!)
v. CaCl availability to allow citrate anticoagulation
w. Easier blood prime process (for those who use blood priming, especially for small infants)
x. More precise volume control when using lower flow rates
y. Simplicity/speed of setup
z. Smaller, less complicated machine than prismaflex
aa. Volume outside of patient
bb. Ability to adjust all flow rates in smaller increments for smaller children
13. What new device or therapy would have the greatest positive impact on the mortality of your patients? Please describe the attributes and incidence rate at your institution.
a. Ability to provide either hemodialysis or CRRT with much lower extracorporeal blood volume and pediatric sized non-AN69 CRRT membrane for the Prismaflex.
b. Crrt peds tubing
c. smaller crrt equipment
d. Blood prime is a big problem so minimizing extracorporeal volume and changing CRRt filter to one that doesn’t have bradykinin release would be the most important advance.
e. Safe CRRT for smaller infants and children without need for blood priming and concern of bradykinin release syndrome.
f. Low flow CRRT for infants with AKI able to scale fluid removal in the smallest possible rate changes 30%– cardiacs and neonates
g. Ability to perform short daily dialysis 5-7 times per week. Honestly this or potentially hemodialfiltration with paediatric specific equipment is most likely to trump all other improvements in technical equipment.
h. Anything preventative is the clear winner – it’s better never to have AKI at all. 2. For established AKI that requires RRT: we need a reliable, accurate, simple, robust CRRT system that is designed specifically to use in the pediatric age/size range, and equally reliable catheters so that we can connect this great new machine to the patient. This would save kids who now die from AKI-related complications, permit therapy in some who never get it because they are “too small”, and would allow greater use of the therapy for support to all critically ill children even with milder AKI.
i. We have difficulty starting PD too early resulting in dialysate leaks. It is best to allow catheter to heal in.
j. We need small HD catheter to allow easy access to HD while PD catheter is healing.
A better 7 Fr double lumen HD catheter and smaller priming volume for CRRT without bradykinin release syndrome
14. What new device or therapy would benefit the greatest number of your patients? Please describe the attributes and incidence rate at your institution.
a. Better infant and neonatal HD catheters and a small CRRT dialyzer that is not AN69
b. Automated citrate.
c. Preventing AKI
d. Smaller crrt equipment
e. CRRT for smaller infants and children Smaller HD lines for those older than neonates, but not large enough for smaller adult lines
A cycler that allowed us to mix solutions in more ways – i.e. create online solutions, change dwell times on each isolated cycle/ a system that could be programmed and interrogated via the Web/Online – thus allowing us to modify nightly runs to achieve specific goals – e.g. remove the extra fluid one night then set up for better PO4 clearance the next….
f. The CRRT machine needs to be thought of as a routine part of critical care, just like the ventilator or the IV pump, not as a last-ditch rescue device.
15. Please describe any device or therapy improvements that have not been addressed by other questions in this survey.
a. Consideration of antibiotic-coated HD catheters
b. Plasmapheresis should be available to neonates
c. Wider range, eg amino acid containing dialysate for PD
d. On-line generation of ultrapure or, ideally, sterile solutions for CRRT to reduce burdens/costs from bag systems
f. Miniaturization of CRRT device – the ICU rooms get very crowded
g. Home PD machines that recognize the low or negative UF we often see in our polyuric children, and allow for more flexible settings
h. More durable PD catheters (some of our patients have waited >5 years for transplant, and the catheters develop holes near the titanium adapter)
i. Careful review of UF control technology – are gravimetric systems really best or would other methods (e.g., volumetric, balancing chamber, flow meter, etc) be superior?
16. Please post any additional comments.
a. Thanks!
b. Even with all the big dreams – if I could just get my hands on what my colleagues outside the US have I could probably help 50-100 more kids at my hospital every year.